Turnaround times – what are we seeing?
Foreword
Managing the ever-growing volume of patient scans is an ongoing challenge for radiologists across the UK, adding additional pressure on our heavy workloads and causing delays in crucial patient diagnoses and treatment.
The Royal College of Radiologists has been working with NHS England (NHSE) to introduce a new target. Starting from August 2023, the national target is that 100% of scans should be reported within four weeks. This initiative helps us to measure and demonstrate the strained capacity within radiology departments for the first time.
Alongside this target, NHSE have published data from the two preceding years, measuring the percentage of scans which took over four weeks for a report to be made available after the scan was carried out. In this article, we have attempted to break down this data and explore what it means for our Fellows and members, as well as for patients. The data shows a complex picture but reinforces what we know to be the case - that a substantial number of patients are waiting far too long to receive their scan results.
The data shows an urgent need for the Government and NHSE to address the challenges faced by radiology departments to meet the new reporting target.
Looking ahead, it is crucial to recognise the dedication and expertise of radiologists, who strive to provide high-quality and timely interpretations of medical images. It is only by demonstrating the situation within which we are working that we can identify the support we need to alleviate the pressures on radiologists – ensuring patients receive the timely care they deserve. We hope that this briefing goes some way in supporting this.
Dr Stephen Harden, Vice President, Clinical Radiology

Diagnostic imaging reporting turnaround time data
Prior to August 2023, the diagnostic data we had available was not good enough to support us in demonstrating the lack of capacity in radiology departments across the country and strengthen the case for investment in radiology. NHS England’s diagnostic waiting time data measures the time from when a patient is referred for their imaging investigation to the test being carried out. While this is important for measuring capacity in certain parts of the system, it is less meaningful for patients, as it fails to include the time until the imaging report is issued and so the diagnosis is made, or the potential condition ruled out.
For some time, The Royal College of Radiologists and NHS England have been working to produce a new dataset which accurately measures the period between an imaging examination and the verified report being made available to the referring clinician. This period is referred to as the ‘turnaround time’ (TAT). Keeping TATs as short as possible, while ensuring adequate time for full and proper assessment of imaging, is important for the timely diagnosis of patients and for bringing down waiting lists.
NHS England have now issued a new target which establishes the maximum length of time within which an imaging report should be returned to the referring clinician. The turnaround time depends on the clinical setting and the patient pathway.
From August 2023, a national target has been introduced for 100% of scans to be reported within four weeks, regardless of the pathway. In the current climate, this target is seen as challenging, but achievable based on a fully staffed department.
This new performance indicator will enable NHS England, regions, and providers to track the performance of the service, especially in the context of chronic workforce shortages. While there will be no repercussions for those that don’t achieve this, the new target can serve as a benchmark, and potentially reinforce the need for further investment in radiologists.
Alongside this new target, NHS England published just over two years of TAT data (April 2021 – June 2023), which records the percentage of reports which were produced beyond the four-week target. To calculate the number of reports produced after 28 days, as NHS England does not publish this data, we have multiplied the percentage of reports ‘>28 days’ by the ‘total cases.’
This briefing looks at this new dataset in closer detail and what it means for our Fellows and members.
What does the data show us?
Large volumes of imaging investigations are being reported beyond four weeks from the time of imaging.
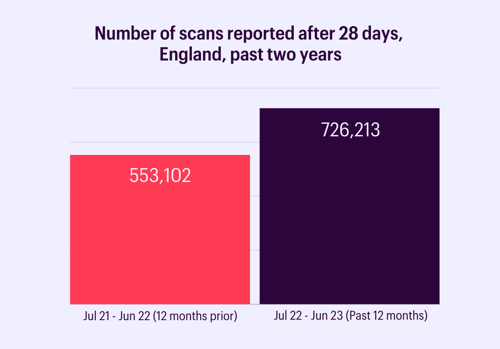
Over the past year, nearly three-quarters of a million patients’ imaging tests were not reported within four weeks.[1]
This has increased by almost 200,000 from the previous year, representing a 31% rise.
[1] This represents 1.7% of all imaging investigations, and a further 5.5% were returned as not known.
When looking at the type of imaging that is almost exclusively reported by radiologists, we see a similar pattern.
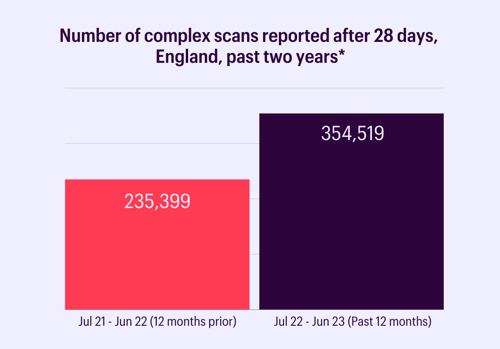
Focusing on the scans that radiologists exclusively report, and therefore take up most of a radiologist’s reporting workload (MRI, CT, PET, and nuclear medicine scans), we see a similar trend.[2]
Last year, over 100,000 more scans weren’t reported within the new four-week target time compared with the previous year. This is a 51% increase, significantly higher than that for all imaging tests.
*Number of CT, MRI, PET, and nuclear medicine scans reported after four weeks, over the past two years (July 2021– June 2023).
[2] This represents 3.1% of all imaging investigations, and a further 6.8% were returned as not known.
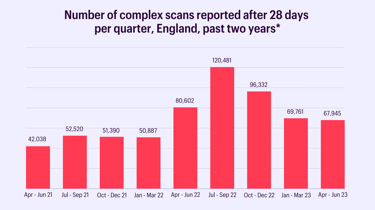
Breaking it down by quarter, the data shows a mixed picture.
The data shows a surge in scans being reported after four weeks from April to December 2022 (Q1 – Q3 2022-23), and in particular from July - September. The causes of this aren’t fully known but may relate to an expected increase related to summer holiday leave and bank holidays. The data would not suggest that delayed diagnoses and long waiting times can be largely attributed to recent industrial action.
For the past six months, just under 70,000 scans each quarter, or approximately 20,000 each month, were reported beyond four weeks, higher than in the period immediately after the final Covid-19 lockdown (July-September 2021).
While it appears the number of scans reported after four weeks may have started to settle, we await the next data release to see if last year’s seasonal variation is in fact a trend.
Demand is outstripping capacity, despite action being taken including the increasing utilisation of in- and outsourcing. Without further efforts to boost capacity, backlogs will continue to grow. With demand only increasing, the picture is unlikely to improve in the short term.
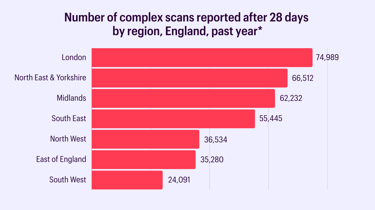
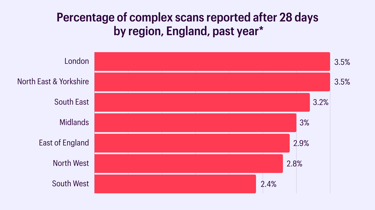
There is regional variation in the number of scans reported after four weeks.
The areas which have a higher number of scans reported after 28 days are broadly reflective of larger population sizes, meaning greater demand for services. The South West, East of England and North West have smaller population sizes hence a lower number of scans reported after 28 days.
The percentage of scans going unreported within four weeks is similar across all regions. London has the highest proportion at 3.5% of scans and the South West has the lowest proportion with 2.4% of scans going unreported within four weeks.
It is uncertain when a sizeable proportion of scans were reported.
When providers submit their TAT data, they have the option to say that it is ‘not known’ when the report was returned. Concerningly, providers could not determine when over two million scans in both 2021 and 2022, and over a million so far in 2023 were reported. This represents between 5-8% of the total number of scans reported.
To improve data collection and help with benchmarking, NHS England should seek to understand the reasons why departments do not know when a scan was reported and support them to provide, and have access to, complete data records. This information should be held in radiology information systems.
So what?
Radiologists’ workload has risen substantially in recent years, in terms of both quantity and complexity. While the rate of CT and MRI scanning activity is rising by more than 5% annually, the radiology consultant workforce grew by just 3% in 2022.
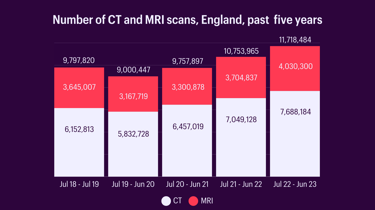
Over the past 12 months alone, the data shows a 9% increase in volumes of CT and MRI scans.
The growth of the radiology workforce is not keeping pace with demand for services. That radiology departments are unable to return scans within the perceived-to-be modest target of four weeks demonstrates the scale of the staffing crisis.
Impact on patients
These shortfalls mean too many patients are having to wait too long for their diagnosis. This has a knock-on effect on all stages of the patient pathway - because of a slow diagnosis, patients may be delayed from either starting treatment or receiving the next stage of appropriate care. There is evidence to show that a patient’s health deteriorates while they are waiting on the pathway, and we know that for every four weeks a patient is delayed from starting cancer treatment, their risk of death increases by approximately 10%.[i],[ii]
Similarly, long waiting periods to receive test results can cause huge anxiety and stress for patients and their families.
Impact on doctors
The data is a clear indication that we do not have enough radiologists to cope with the level of demand for imaging services. Chronic workforce shortages are preventing the delivery of a timely and effective service.
Increasingly, our members are reporting that they are unable to address the workload. In our 2022 workforce census, only 1 in 4 clinical directors said they had enough radiologists to deliver safe and effective patient care. 98% of clinical directors are concerned that workforce shortfalls will result in backlogs and delays. In 2022, there was a 29% shortfall of clinical consultant radiologists, which is expected to rise to 40% by 2027.
Radiologists are working under extreme pressure to keep on top of reporting requirements, and this will further contribute to a fatigued workforce with an increased risk of burn-out. In 2022, 100% of clinical directors said they were concerned about staff morale and burnout in their department.
This also impacts our ability to train future generations. Insufficient staffing levels mean that radiology departments are unable to free up resources for training, worsening the situation now and for the future.
Novel technologies and AI may help support radiology turnaround times but will also fail to fulfil their potential if doctors do not have sufficient time for their thorough evaluation, in addition to completing their clinical work.
Bringing down waiting lists is a national priority, set both by the Government and NHS England, but without investment into radiology departments and action to increase the number of doctors reporting scans, this will not be achieved.
Next steps
From August 2023, the target is that no verified report should take longer than four weeks after image acquisition, under any circumstance. There is little chance of improving where we are now without investment in radiology.
This target is also considered a stepping stone to more ambitious TATs (2 weeks) in the future. If we have any hope of moving to this new target, let alone meeting the current one, we simply need more radiologists.
Recommendations
To support this ambition, NHS England and the Department of Health and Social Care should:
1. Grow the workforce by sustaining the increase of radiology specialty training posts
- Recognition that early diagnosis is critical to improving patient outcomes means that we will continue to see a higher demand for imaging services and radiologists in the future.
- To meet this demand, we need to train more.
- Trainees, particularly as they become more senior, bring significant benefits to departments, contributing vital reporting capacity and reducing the need for outsourcing.
- Recent increases in training places should be sustained, even if not all departments are able to take all their extra posts every year.
2. Expand training capacity, both in terms of doctors’ capacity to train and physical space
- To facilitate an increase in training places, we need an urgent focus on expanding capacity to train.
- A lack of capacity to train new doctors may prevent a department’s ability or willingness to take on new trainees, despite their proven ability to support services.
- This includes physical space to teach, and the consultant’s time to spend on training. Currently, clinical pressures inhibit radiologists’ ability to protect time for supporting professional activities (SPAs) including training.
- We need to prioritise training, including protecting SPA time in consultants’ job plans and exploring additional capacity such as encouraging recently retired doctors to return to deliver training.
- Funding for imaging academies should be protected to continue to train the next generation. Additional funding will be required to facilitate an increase in trainees.
- To incentivise all departments to take on trainees, the Government should review how training posts are currently funded with the aim of simplifying the process.
3. Improve working conditions to stem the flow of doctors leaving the system
- Between 2020 - 2022, the median age at which a clinical radiologist retired dropped from 58 to 51.
- To keep up with the rising demand for diagnostics, keeping experienced and highly skilled radiologists working in the system must be a priority.
- Trusts and health boards should take active steps to improve doctors’ day-to-day working conditions to make sure they feel valued by their employers. This should include employing sufficient administrative staff to support doctors, exploring flexible working patterns, and providing access to rest spaces and food and drink.
4. Invest in IT systems and networks to support radiologists’ ability to report scans
- Radiologists critically need reliable and fast IT systems, physical equipment, and supportive infrastructure to carry out their jobs.
- Slow and cumbersome IT systems can be frustrating, increasing stress on doctors, reducing reporting capacity and efficiency, and producing poorer patient outcomes due to delayed diagnosis.
- The Department of Health and Social Care should support trusts and health boards to invest in improved IT infrastructure and systems for radiologists.
5. To support the continued monitoring of radiologists’ capacity, NHS England should also invest further in the TAT dataset
- Currently, the data only allows us to monitor the total percentage that is reported after four weeks. Reporting on the number of scans, as well as percentages, would improve the quality of the dataset.
- The TAT guideline also includes specific targets for each of the different patient pathways. For instance, for patients on the 28-day faster diagnosis standard pathway, their scan should be reported within three days.
- In the future, the data should be able to show whether these individual targets are being achieved.
- Similarly, to strengthen the dataset and help with local benchmarking, NHS England should seek to understand the reasons why departments are returning ‘not knowns’ and support them to provide complete data.
This data is also available at provider and network levels. If you would like any further detail on the data or have any questions, please contact [email protected].
[i] Care Quality Commission. 2023. Adult inpatient survey 2022. Available at: https://www.cqc.org.uk/publications/surveys/adult-inpatient-survey. [Accessed November 2023].
[ii] Hanna T P, King W D, Thibodeau S, Jalink M, Paulin G A, Harvey-Jones E et al. Mortality due to cancer treatment delay: systematic review and meta-analysis BMJ 2020.